Post Trauma: When Emotional Wounds Penetrate the Home

An interview with Prof. Rachel Dekel from the Dangoor Center and the School of Social Work at Bar-Ilan University on the impact of trauma on relationships and family.
“Anger, conflict, and outbursts are an inseparable part of trauma. We see it in supermarket lines, on the road, and also within families—and there is a lot of shame and guilt around it,” says Prof. Rachel Dekel of the Dangoor Center for Personalized Medicine and the School of Social Work at Bar-Ilan University. “Mothers and fathers of soldiers also feel anger. If I have a son in the army and I am full of worry—that worry may come out as anger.”
Prof. Dekel researches the impact of traumatic events on families and couples. For nearly three decades, she has studied and taught a range of topics related to trauma coping. Together with partners, she initiated the “Ripples of Recovery” project, which offers interventions, training, and research from a family-centered perspective, including couples therapy when one or both partners are experiencing post-traumatic distress. Both her theoretical research and fieldwork highlight the importance of a supportive couple and family network in the face of trauma. The flipside, however, is that the trauma takes a toll on those closest to the individual, making it necessary to move beyond individual-focus treatment.
She begins with a story. “I recently read in the newspaper about a woman who was evacuated to a hotel with her daughter, who had just finished first grade. A classmate sent her a voice message and asked if she was coming to school. ‘I’m a friend and you’re a friend, and together we’re a pair—and a pair together can beat anything,’ he told her.”
That’s remarkable. That child managed to articulate your very approach—that the one affected is not alone, that they are part of a system.
“Our approach is ecological. We believe that traumatic events have an impact on spouses, the family, and the community—for better or worse. You can see it now with the wives of reservists, for example. Just like that boy said, the power of the couple can help in coping with trauma, but the trauma can also deeply harm the partner. We’re conducting a large study on the couple dynamics of reservists suffering from trauma, in which we examine the conditions under which the partner’s distress rises—so both partners are in distress—and when one of them is able to lower it. We work extensively on anger, studying its dynamics within the couple to understand how to help the couple, the family, and the parents.”
How do you study that—through questionnaires?
“Not only. We have a treatment-research project that includes many forms of measurement, not just questionnaires and in-depth interviews, but also physiological metrics like blood pressure and heart rate. Our goal is to see ‘beneath the skin,’ beyond what people report—to understand how partners actually react to each other and under what conditions there’s a positive response to treatment, in order to identify the most effective way to achieve both individual and relational regulation.”
So you're trying to measure unspoken anger.
“Anger, conflict, and intimate partner violence. According to another study we’re conducting, since the start of the war there’s data indicating a rise in relationship conflict due to prolonged reserve duty. Communication often diminishes, and it’s hard for reservists’ wives to admit they’re angry too. We’re seeing a rise in conflict, anger, and sometimes violence. We’re running a project on the prevention of domestic violence with about 70,000 participants in Beit HaLochem centers across the country. The data shows an increase in couple conflict linked to reserve duty, and a connection between psychological state, post-traumatic distress, and anger—one of the key symptoms of PTSD.”
“The syndrome is not uniform. It may be accompanied by depression, sleep disorders, and addictions. That is why both diagnosis and rehabilitation must be personalized.”
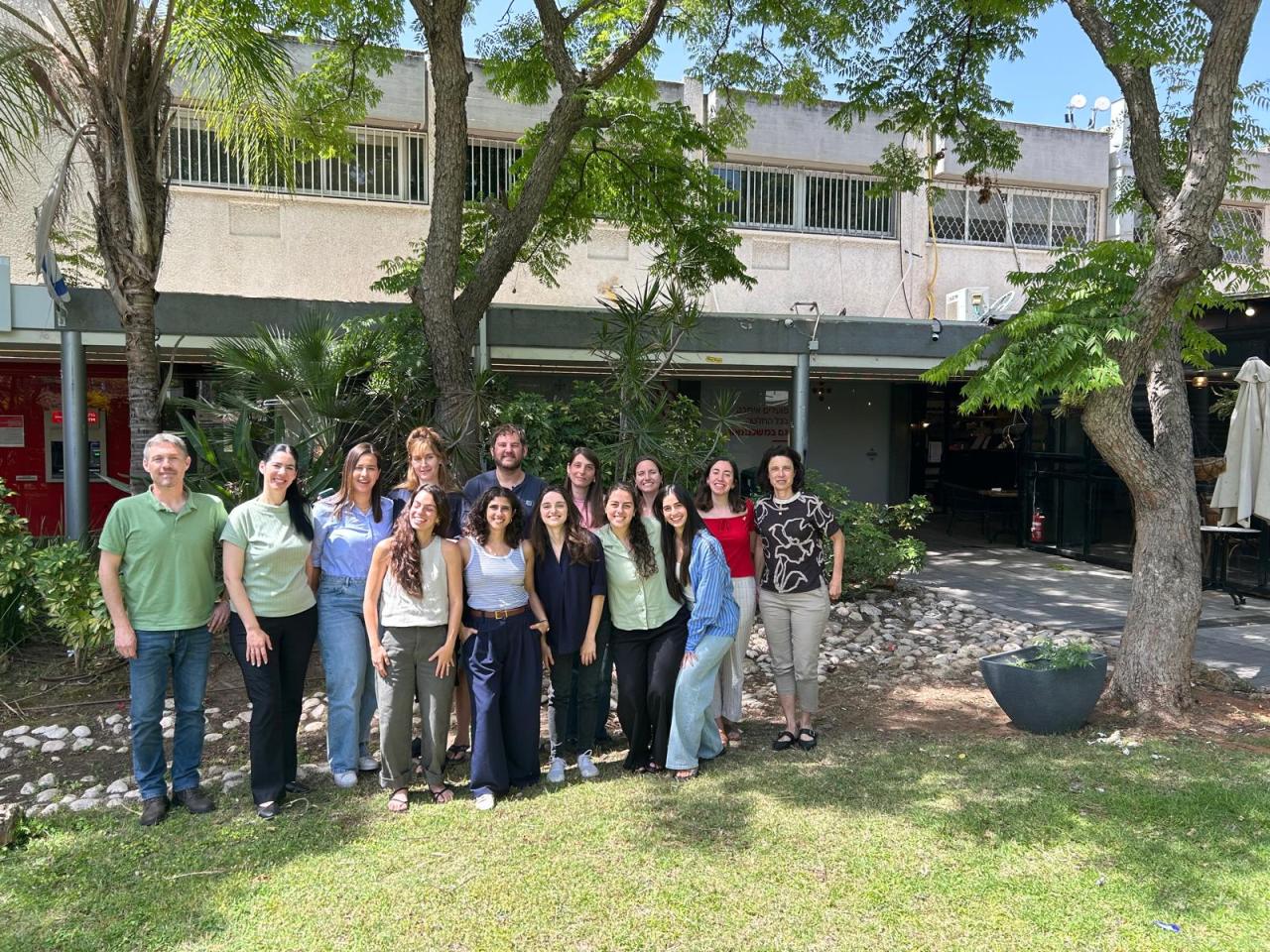
 From a couples’ retreat
From a couples’ retreat
Women Seek Help Less Often
How has the war changed patterns of trauma, anger, and violence?
“We have data from studies conducted before and after the war, and what we’re seeing is a different kind of violence than what we’ve known—first and foremost because we’re now seeing violence in families that had no prior history of it. In the past, broadly speaking, we dealt with domestic violence rooted in fear and control—the need for surveillance and hierarchy. Today, we’re seeing more violence stemming from an inability to regulate the body and emotions, difficulty transitioning from the intensity of reserve duty to everyday life.
A reservist comes home and asks himself: What am I doing here? What’s the meaning of what I’m doing? For example, why should I be the one bathing the children? Even the transition from bomb shelters back to routine is not easy—physically or emotionally. It’s a shift between extremes, and it takes the body and mind a long time to readjust from high alert back to normal life and vice versa.”
In one of your studies, you also found differences between men and women in their response patterns. Can you tell us about that?
“The data show that the percentage of women serving in the reserves has risen to 30%, but the percentage of women seeking help after reserve duty has not increased—which means there is a gap. Even though women are now serving five times more than in the past, their share among those seeking help remains just six percent. How do we explain that? We know that it’s not only the experiences they go through that are different, but also how their partners, families, and society relate to their service. Sometimes they’re told, ‘You wanted this, you chose it.’ Part of the lack of help-seeking reflects resilience and coping, but part of it may also be requests that have not yet come—or will come later.”
And when they do need help, who do they turn to?
“Our study is qualitative, meaning it’s based on interviews, and we heard from the female reservists we interviewed that there’s a hierarchy of ‘combat-worthiness’ even within their relationships. Reserve duty doesn’t always strengthen the relationship—sometimes the opposite happens. We found that many times, when women need support related to the stress of war, they turn to friends rather than their partners. Is that because there’s tension between the couple over who contributed more, who’s more resilient? Is it because the partner is busy with his own reserve duty? We’re currently analyzing the data. The study is still small, but it’s an important question.”
Parents Are Taking on Too Much
A surprising angle is that of the parents of reservists. They too are affected.
“Yes, many of the soldiers and reservists are young adults in their twenties or thirties, where they’re supposed to begin building independent lives—studying, working, and visiting their parents maybe once every week or two. But because of the war, we’re seeing more and more of them returning to their parents. Sometimes it’s due to relationship crises, or because they’ve just finished school and the war put a halt to their progress. So the parents are in distress.”
“Their 30-year-old child has a high fever.”
[a line from an Ehud Banai song]
“Exactly. We need to remember that when a child is suffering from emotional distress, and they’re not willing to talk to you, and you can’t force them into treatment, the parents are also suffering. We’ve seen parents of married children helping care for their grandchildren because they fear the daughter-in-law will leave if the burden is too much. Some are handling their kids’ psychiatric medications, cleaning their rooms, and taking care of their obligations. They do it willingly and with good intentions—but if they keep doing it for them all the time, they’re not actually helping.”
So the conclusion is not to take on too much?
“There are studies on PTSD that show the greater the distress, the more partners tend to make ‘adjustments’—and the more adjustments they make, the more the traumatic distress of the partner increases. Why does this happen? Because if, as a partner, I take the kids to preschool instead of him, I’m actually reinforcing his avoidance and his lack of control over his life. What starts as a well-meaning act ends up strengthening the avoidance cycle. The same goes for parents who take on too much. The son tells himself: maybe I really can’t.”
Even though it's done with good intentions.
“Of course. But what initially helps and lowers the anxiety levels of the family member with PTSD ultimately increases avoidance and prevents a return to functioning. In an ongoing study, we guided several groups of mothers of Nova survivors—some of whom shared that after the trauma, they left everything behind to care for their adult children: cooking for them, cleaning up after them. The parents tell themselves, ‘If I don’t do it, who will?’ But despite their good intentions, this behavior can actually perpetuate the condition. They become a barometer for their children, signaling to them that they are incapable of caring for themselves.”
Personalized Rehabilitation
What exactly is post-trauma? It seems to include a huge range of symptoms.
“There are different types of post-trauma. In one article I saw a figure mentioning over 60,000 patterns. That means it’s not a single phenomenon. Some people become more extroverted, angry, and impatient; others withdraw, shut down, and become extremely avoidant; and some are both.”
How can you build a treatment system for a condition with such varied expressions?
“That’s precisely why our research is part of personalized medicine. Both the diagnosis and the rehabilitation must be tailored to the individual. The syndrome isn’t uniform—it may be accompanied by depression, sleep disorders, and addictions. And I’m not just talking about drugs, but also addictions to pornography, shopping, or gambling. Sometimes there is intimate partner or family violence. So the consequences of the war are extremely broad, and we need to be prepared to recognize the full spectrum and ask the right questions when someone seeks help.”
Last Updated Date : 04/11/2025