Brain Cancer: Communication Between Tumor Cells and Surrounding Cells Is Critical for Diagnosis, Treatment, and Cure
Professor Chaya Brodie, from the Dangoor Center for Personalized Medicine and the Faculty of Life Sciences at Bar-Ilan University, is developing new approaches to treat aggressive brain cancer — research that may also advance therapies for other diseases such as ALS and Parkinson’s.
“I work on serious diseases that don’t always have a prospect of recovery. Although our ultimate goal is a complete cure, we also aim to develop treatments that can turn these severe diseases into chronic conditions — like diabetes or heart disease — allowing patients to live with dignity and a good quality of life.”
Can the most aggressive form of brain cancer be transformed from an incurable disease into one that can be managed and treated? That is the aspiration driving Professor Chaya Brodie.
Professor Brodie studies glioblastoma, a particularly aggressive brain cancer, and her findings are influencing research and diagnosis across other conditions, including Duchenne muscular dystrophy, Parkinson’s disease, and ALS.
“Glioblastomas are the most aggressive primary brain tumors,” says Professor Brodie. “They are resistant to nearly all existing treatments, including radiation. For decades, the average life expectancy after diagnosis has remained around 14–16 months — and unfortunately, despite significant progress in research and medical technologies, this has not substantially changed.”
 Prof. Chaya Brodie
Prof. Chaya Brodie
Why Is It So Difficult to Treat Glioblastoma?
“These tumors are embedded in the brain and can spread to different areas, making it impossible to remove them completely without damaging brain function. Many drugs also fail to penetrate the brain effectively due to the blood–brain barrier, which limits the entry of substances. In addition, these tumors are extremely heterogeneous, which complicates treatment. Brain tumors contain two main types of cells: the tumor cells themselves and the cancer stem cells. It is these stem cells that drive tumor recurrence and resistance. For example, after irradiation, even if the number of tumor cells decreases, the number of cancer stem cells increases. Most current treatments target the tumor cells, not the stem cells, which is why they struggle to eradicate the disease.”
Which cells are you focusing on in your research?
“In addition to cancer stem cells, we are working on the communication between tumor cells and cancer stem cells, or between them and other cells in the environment, communication that is critical for the tumor’s ability to grow and to develop resistance to various treatments. This communication takes place through substances secreted by the tumor, including exosomes, which are tiny extracellular vesicles — that is, small bubbles measuring only a few dozen nanometers—that store within them a wide variety of molecules. The cell knows how to release these molecules so that they reach the bloodstream and other cells as needed, and uses them for intercellular communication.”
And are you examining what’s inside these vesicles?
“Yes, through the vesicles’ contents, we can understand the cell’s ‘intentions.’ If the cell wants to promote its growth, it releases molecules that influence its environment to support it. If it wants to suppress the immune system, it uses a different molecular ‘language.’ In some cancers, vesicles even prepare distant tissues for metastasis. Although brain tumors don’t form metastases in other organs, they similarly spread within the brain, and this process is linked to vesicle activity.”
And all this takes place outside the tumor cells themselves.
“Exactly. That is why a cycle is created of cells in the tumor’s environment that support it, and if we do not break that cycle, it will continue to thrive. In other words, if we find a drug that works only on the tumor cells, we will solve only part of the problem, or the tumor will come back. We must also treat the tumor’s environment, the stem cells, and the extracellular communication.”
 An innovative treatment for Duchenne muscular dystrophy
An innovative treatment for Duchenne muscular dystrophy
What is the role of extracellular vesicles in the disease?
“Let’s take Duchenne muscular dystrophy as an example. It’s a genetic disease, but it also progresses through secondary processes mediated by vesicles circulating in the bloodstream. These vesicles carry cargo that promotes disease progression. In a study we conducted with Professor Sivan Korenblit, we found that when vesicles from Duchenne patients were placed on worms, the worms developed signs of muscle degeneration. Similar results were observed in zebrafish, in collaboration with Professor Krasik from the Faculty of Medicine in Safed. Likewise, when vesicles from ALS patients were applied to healthy nerve cells, those cells began to degenerate. This shows that it’s not only the genetic mutation causing nerve cell death, but also the vesicles themselves. Therefore, to treat these diseases, we must target both the primary cause and the harmful signals transmitted through vesicles.”
Do you also use extracellular vesicles to diagnose diseases?
“Typically, to determine the type of cancer, we usually perform a biopsy, but it’s not always possible to access the tumor. This led to the development of the ‘liquid biopsy’, which analyzes bodily fluids such as blood, urine, or cerebrospinal fluid. These contain extracellular vesicles secreted by tumors. Unlike many other molecules that degrade quickly, vesicles are remarkably stable, allowing us to obtain a clear picture of what’s happening in the body.”
Does this research have applications?
“We collaborate with research labs and pharmaceutical companies to identify markers in blood and saliva samples that can help monitor disease progression and patient responses to treatment. Our work focuses on diseases including Duchenne muscular dystrophy, amyloidosis, Parkinson’s disease, and multiple sclerosis.
“Beyond diagnostics, vesicles themselves may become therapeutic tools. Because they can efficiently deliver drugs, we can load them with medications and send them directly to target cells — an approach known as exosome therapy.”
 Personalized models of brain tumors
Personalized models of brain tumors
Replicating the Tumor with AI and 3D Models
How does artificial intelligence help you?
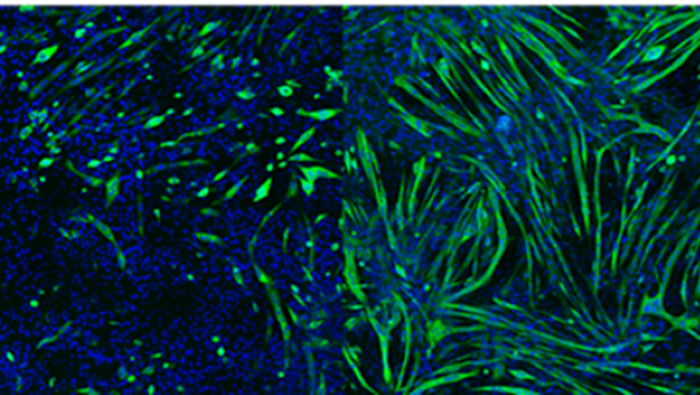
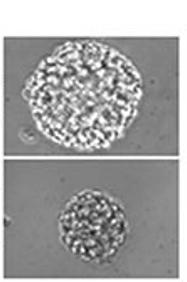
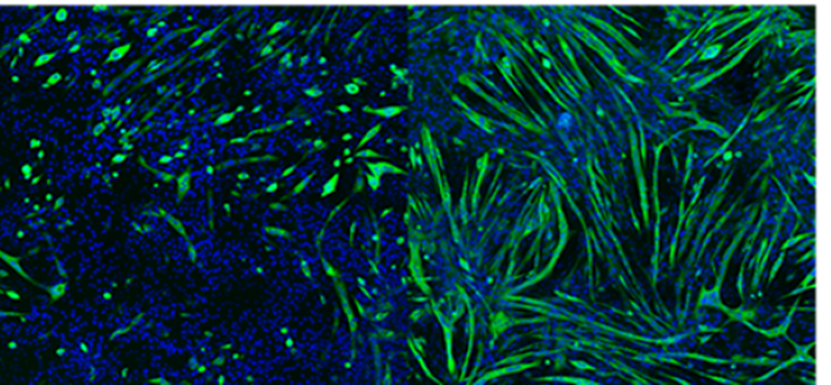
“We can’t study all of the different types of existing tumors in the lab, so we use databases that include surveys of hundreds of tumors and focus our questions accordingly. The combination of bioinformatics with the ‘wet lab’ is what makes our work unique, and it allows us to work more efficiently and to ask the questions that lead us to new genes or mechanisms that have not yet been studied. We build unique models based on three-dimensional cultures. Unlike regular cultures that grow in a two-dimensional dish, these cultures preserve the original characteristics of the tumor.”
Why is it important for the tumor to be in a three-dimensional culture?
“To understand the processes that take place inside the tumor and the connection between it and its environment. The three-dimensional tumor is closer to the way the tumor exists in the brain, and the more we build it to resemble the tumor in the brain, the closer the insights we gain will be to reality.”
Part of your research involves testing old drugs on new diseases.
“This research direction is called drug repurposing, finding new therapeutic uses for existing drugs. Every drug—as can be seen in the leaflet that comes with it—also has effects beyond the purpose for which we take it. Since the development of a new drug is a long process and involves enormous costs, it has become common today to examine whether drugs already approved by the FDA can also treat other diseases, in addition to the original ones for which they were intended.”
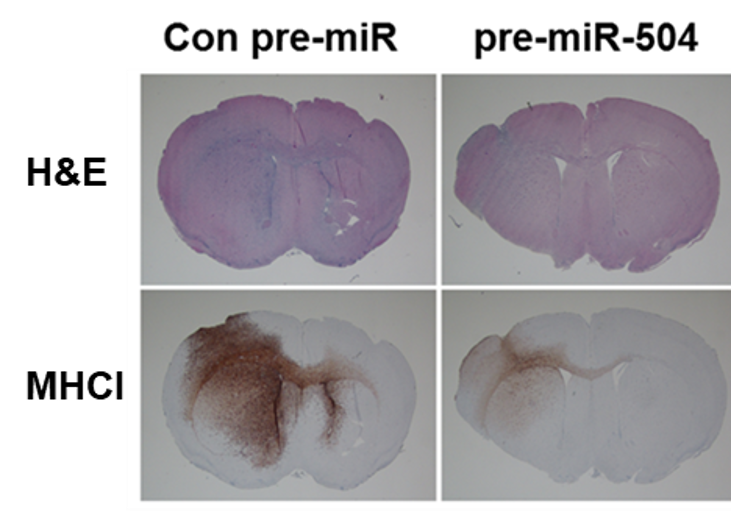
 Metformin, a diabetes drug, reduces the growth of cancer stem cells in glioma
Metformin, a diabetes drug, reduces the growth of cancer stem cells in glioma
Can you give an example?
“There is a drug for type 2 diabetes called metformin, and it was found that diabetic patients who took it had a lower chance of developing cancer, even though people with diabetes usually have a higher likelihood of developing tumors. In other words, diabetic patients who took metformin had fewer cancers, even compared to healthy individuals. The conclusion was that this drug also has a very significant anti-cancer effect, and it turned out that it has anti-cancer effects in a wide range of tumors. In addition, it was recently discovered that certain anesthetic agents, such as propofol, also have anti-cancer effects, and that using them can help slow the return of the tumor after surgery.”
What about drugs that have problematic side effects?
“Sometimes those are examined as well. There is a well-known drug called thalidomide that was given in the 1950s to pregnant women, but then children were born without limbs, and the drug was withdrawn from the shelves. Yet it turned out that this drug works very well in treating certain types of cancer. Sometimes it is possible to take drugs that were once considered harmful and redirect them to treat a different problem.”
Human Excellence
Professor Brodie completed her Ph.D. at Bar-Ilan University, followed by a postdoctoral fellowship at the University of Colorado, where she conducted research at a university hospital. She later returned to Israel with an Alon Fellowship and established her own lab at Bar-Ilan. Over the years, she has received numerous awards and grants — including funding from Volkswagen, Teva, the ISF, BSF, and the McDonnell Foundation.
Why did you return to Bar-Ilan?
“I was indeed offered a position at the University of Colorado, but I come from a very Zionist family, and I am the only one in my family who lived abroad. My whole family is here, and we wanted to come back to Israel. I chose Bar-Ilan, which is characterized by a combination of excellence and humanity.”
How is this reflected in practice?
“I grew up in a family of psychologists and educators whose guiding belief was that everyone should be included - including those with special needs. I believe excellence is not only scientific but also human. Our role as lecturers and researchers is to help people progress, even if they aren't the most academically outstanding. Bar-Ilan embodies this value."
Do you apply this in your own laboratory?
“I give space to people of all kinds. I don’t believe grades say everything. I have had many students who, at first, were not accepted elsewhere, and today they are a significant and contributing part of the scientific community. A few years ago, a student with ADD came to Bar-Ilan, and when I asked him why he chose this university, he said: At other universities I was different, but here I’m special.”
What is the role of the Dangoor Center and of personalized medicine in your work?
“The idea of personalized medicine is crucial. Tailoring treatment to each patient is essential for developing approaches that allow people to live with their disease - even without a full cure. Large-scale studies are important, but there's also tremendous insight to be gained from individual cases."
The academic world is relatively male-dominated, especially when it comes to senior faculty. Do you feel that yourself, particularly as a researcher from the religious sector?
“Today, the situation is much better, and there are many women researchers in the faculty. When I went to Colorado for my postdoc, I was the only woman in a lab of 18 men. But I didn't feel treated differently. I also faced questions about my religious observance, since few women in my field were religious. Still, I never felt my faith stood in my way.
Has keeping tradition not been an obstacle for you?
“I come from a very special family that combines Torah and science, and I don’t feel that my faith has hindered my career. Sometimes it makes things more difficult, because as someone who observes Shabbat, I cannot always take part, especially not actively, in conferences that are held on Shabbat or holidays. Once, at a conference that took place on Shabbat, I couldn't use a microphone or projector, so I presented without them. The audience sat in complete silence, and my colleague advanced the slides at just the right moments. In the end, people respect you for staying true to your principles."
 Looking ahead: advanced cell cultures enable the development of innovative treatments
Looking ahead: advanced cell cultures enable the development of innovative treatments
On a personal level, what other dreams would you like to fulfill as a scientist?
“A scientist always has dreams. One dream is to be able to keep up with the pace of the scientific world, which is developing so rapidly and where the innovations are sometimes very dramatic. I wish for myself the ability to integrate these innovations into my own research. A second dream is to succeed in making an impact and helping others. It is said that if you save one life, you save an entire world. My daughter is a doctor, and she treats people every day. For us as researchers, it is harder to say whether our work has helped patients in a practical sense, so I hope my research will succeed in helping people. And even if we don't achieve a complete cure, perhaps we can turn incurable diseases into chronic ones - allowing patients to live full, dignified lives. For me, that would be an extraordinary achievement."
Last Updated Date : 05/01/2026