“In the coming decade, we expect to see major changes in cancer treatment”
An optimistic interview with Prof. Cyrille Cohen from the Dangoor Center for Personalized Medicine on the tremendous advancements in immunotherapy for cancer and the likelihood that his research will reach patients in the near future.
How might immunotherapy open new avenues for cancer treatment? We met with Prof. Cyrille Cohen from the Dangoor Center for Personalized Medicine, head of the Laboratory for Cancer Immunology and Immunotherapy, to learn about innovative research based on genetic engineering of the immune system and the hottest topics in biotech and medical research. And yes, also here artificial intelligence is changing the rules.
First of all, what’s innovative about the approach of immunotherapy treatments for cancer?
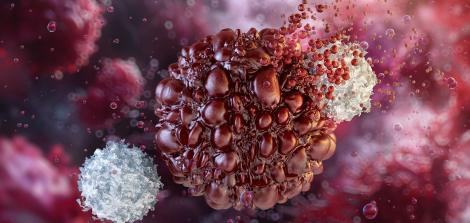
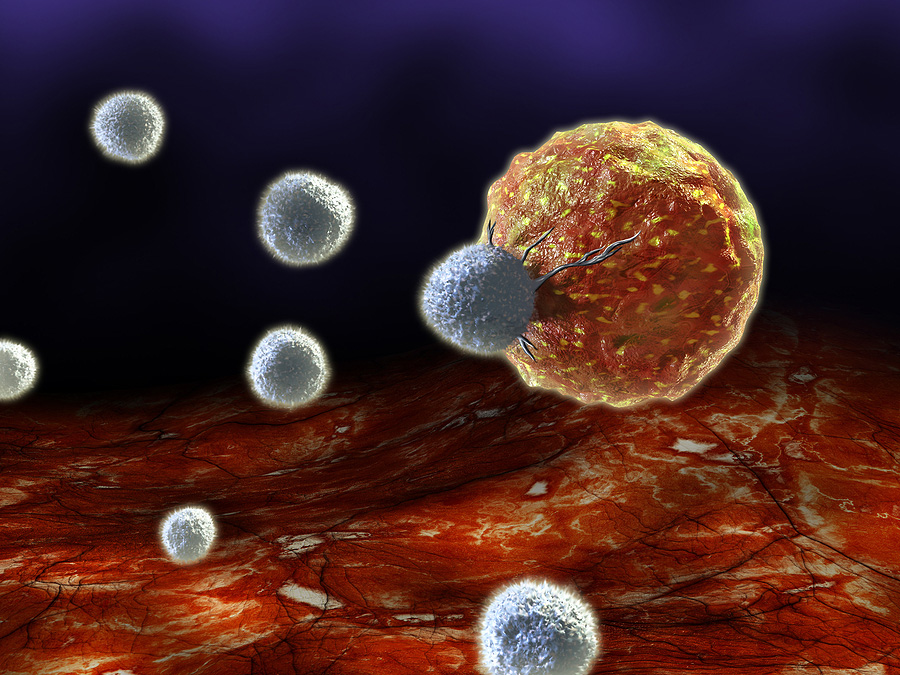
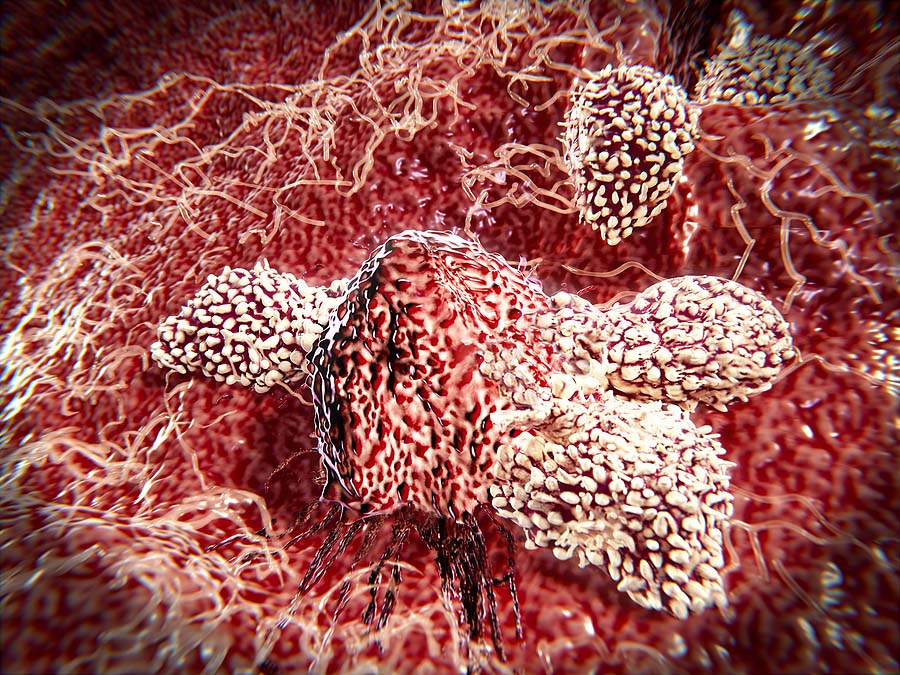
“The fundamental understanding was that cancer is caused by cells that undergo mutations, but the changes are not significant enough for the immune system to distinguish between a normal cell and a cancerous cell. In other words, the prevailing view for many years was that the immune system is not relevant when it comes to tackling cancer. But later, evidence accumulated that the immune system, particularly T cells, contains highly precise detection mechanisms that can indeed differentiate between normal and cancerous cells.”
In other words, the immune system is aware of cancer.
“Yes. T cells can identify a cancerous cell, and they can do so effectively. They are able to recognize it even when cancer manifests through a change of no more than a few atoms within the cell. If we compare the cell to a packed football stadium, in a cancerous cell, two people in the crowd are replaced – that’s all. And this tiny change is enough for a T cell to detect it as cancerous. T cells have an incredible diagnostic power at the molecular level.”
So what goes wrong with the immune system? Why doesn’t it eliminate cancer cells?
“That’s exactly what we’re trying to understand. We’re trying to figure out what goes wrong in the immune system when there’s cancer. We know that sometimes our immune system gets confused and attacks body cells in autoimmune diseases, so the immune system has a set of restraint mechanisms. We also know that cancer cells can use the immune system’s restraint mechanisms to act against the body. Some cancer cells even directly suppress immune activity, for example, by consuming all the available nutrients in their environment, leaving T cells without the ‘rations’ they need to fight cancer. Competition for resources, immune suppression – these are some of the strategies cancer uses to thwart the immune system.”
What are you doing to strengthen the immune system?
“My lab at Bar-Ilan is involved in several research directions in the field, working from the molecular level up to collaborations with hospitals to apply our findings. Some of our developments are already in the clinical trial stage in Israel. For instance, we’re developing protein receptors that enable the immune system to detect changes in cancer cells and help activate the immune response. Recently, we published a study on changes in the sugar levels on the surface of cancer cells. In other words, we discovered that the sugar composition on cancer cells changes to help them evade the immune system, and we can direct the immune system to recognize and respond to these changes.”
How can we act against these sugars that neutralize the immune system?
“These are sialic acid sugars that suppress immune function. We took the natural receptors in the immune system and modified their structure so that now, instead of suppressing the immune system, these sugars activate it. You can think of the immune system as a car, with the cancer cell pressing on its brake – so we swapped the gas and brake pedals, and now, when the cancer tries to press the brake, it actually activates the T cells. That’s one example. There are others.”
What do we do with cancer that consumes sugar?
So please, tell us about another example.
We know that cancer often consumes a lot of glucose and doesn’t leave enough nutrients for immune system cells. How do cancer cells do this? They import glucose into the cell using special pumps, and they accelerate the work of the machines that process the sugar into energy. We said, let’s copy what the cancer cells are doing and replicate the same mechanism in the immune system. So, we equip immune system cells with the same tools and enable them to acquire abilities that are similar to what happens in cancer, so they have the ability to compete with cancer cells and steal the sugar found in their environment.”
And does it work?
“So far, in the experiments we’ve conducted in test tubes and animal models, we’ve shown that T cells engineered with these changes handle cancer much better. They succeed in pulling in the sugar, processing it, and generating energy in a way that enables them to better combat cancer cells. We’re now trying to understand if there are additional traits we should equip the immune system with to help it cope more effectively with the challenging conditions of nutrient scarcity.”
Is there clinical evidence that it works?
“In a previous study, in collaboration with a team from Hadassah Ein Kerem Hospital led by Prof. Spatansky, we created a molecule that both recognizes cancer cells and activates T cells. We introduced this molecule, using a virus, into the T cells of patients with myeloma and amyloidosis (a hematologic disease where blood cells produce defective protein). The response rate among myeloma patients reached 90%, and the response rate among amyloidosis patients was total – 100%.”
What is the advantage of using a virus to enter a T cell?
“Viruses enter cells in the most efficient way possible. We use non-dangerous viruses that can’t replicate; they simply act like a USB drive to transfer information. Sometimes, we also use genetic editing systems like CRISPR, which we learned from bacteria, adapting them for therapeutic purposes and to transfer information between immune cells. Today, non-viral approaches are also being developed, but many of these developments are based on the tools we’ve established with viruses.”
Are the insights you discovered in your research limited to myeloma (a type of blood cancer), or are they relevant to other types of cancer as well?
“We do indeed ask ourselves why cellular immunotherapy works better with blood cancers. It likely relates to the fact that immune cells move through the blood, which provides access to nutrients and oxygen. When there’s a tumor elsewhere in the body, the immune system has to penetrate and survive within it without nutrients, which is a challenge. We are currently working on research across several types of cancer. The challenge for cellular immunotherapy over the next decade will be to transition from blood cancers to other cancers, which make up 85 percent of all cancer cases.”
Organ printing and cultured meat
Prof. Cyrille Cohen was born and raised in Marseille, made aliyah at age 17, and completed his doctorate at the Technion. After his postdoctoral work at the National Institutes of Health in the United States, he turned toward T cell research and joined The Mina & Everard Goodman Faculty of Life Sciences at Bar-Ilan University. He has won numerous awards, including the Knesset Young Investigator Award, the Rothschild Postdoctoral Fellowship, the Gutwirth Award in 2003, the Alon Fellowship for Outstanding Scientists in 2007, recognition from the American Institute for Cancer Research in 2013, the Excellence Award from the Israel Cancer Association in 2013, as well as teaching and research awards from the Technion, Bar-Ilan University, and the National Institute of Health in the U.S.
In his public roles, Prof. Cyrille Cohen serves, among other things, as the outgoing president of the Israel Cancer Research Association. He is a member of several Ministry of Health committees for the approval of clinical trials in advanced therapies, and in 2023, he was appointed Head of the Field of Medicine and Biochemistry at the National Academy of Sciences, which allocates financial grants to researchers and is a highly influential body in Israel’s academic development.
As someone at the Israeli Academy of Sciences responsible for funding research, what do you think are the hottest fields in biology and medicine?
“One of the most fascinating fields, in my opinion, is synthetic biology, which includes, for example, organ printing – it’s amazing to me. Another intriguing field is food tech – the possibility of finding food solutions like cultured meat, which will soon significantly change our diet. Other prioritized research areas are related to our efforts to address sustainability and climate. These are the topics at the forefront. And, of course, we must always prioritize finding solutions for both common and rare diseases.”
How many more years do you think it will take to see these treatment methods in the clinic?
“These fields move relatively quickly. When I opened my lab 17 years ago, I set a goal to reach patients within 10 years. It took us a bit longer – 13 years – but I’m very happy that some of our developments have already reached patients. I can’t specify an exact number of years, but I estimate that in the coming decade, we’ll see major changes in our approach and the tools available to us against cancer, partly due to the rapid development of AI, artificial intelligence. It will be a gradual process, but we’re constantly advancing, and new treatments and drugs that will be real game changers will enter the field.”
What do you expect will happen to cancer in a few decades? Will it become a “chronic” disease?
“I’m optimistic. But my optimism is like that of a marathon runner – it can’t provide immediate solutions, and meanwhile, people die of cancer every day. The progress through immunotherapy is significant, much more than in the last 50 years. I’ve encountered cases of patients who, 20 years ago, were terminally ill, and after being treated with advanced methods, they are still alive. But immunotherapy doesn’t help everyone. Almost every day, I receive requests from cancer patients seeking immediate solutions, and I don’t have any; I’m a researcher and don’t treat patients directly. It’s very frustrating that we still don’t have a cure for cancer. A tremendous effort needs to be invested in cancer prevention and early detection. What we do in the labs is always the last resort. Investment should go into proper education, eliminating smoking at all costs, avoiding unhealthy food, encouraging physical activity, and reducing alcohol. If we do this, we can statistically reduce cancer cases by 40–50 percent.”
Did COVID-19 advance this field of research?
“Very much so. During COVID-19, there was a strong emphasis on the potential of applied advanced biology, which enabled the development of vaccines that saved hundreds of thousands of lives in record time. The COVID vaccines showcased the immense potential of biotech, alongside the scale of biological threats, as a tiny virus was able to disrupt the entire world. We saw that humanity was able to respond, but such threats are constantly present, as there are dozens more families of pathogens around us.”
What makes your research part of personalized medicine – what is “personal” about it?
“Some of the tools we develop are suitable for certain types of patients but not others, and our vision is to create toolkits that allow a doctor to tailor the right treatment to the specific type of tumor and engineer the patient’s own immune system to help it fight effectively.”
Why did you choose to base your lab and career specifically at Bar-Ilan University?
“Bar-Ilan University offers a professional yet close-knit work environment, benefiting from investments in research infrastructure and advanced, high-quality equipment, all of which allow us to test treatments effectively. Thanks to Bar-Ilan’s locations in central Israel and the Galilee, we can also collaborate with several hospitals. I definitely believe that in the coming years, thanks to investment in resources and the support of the administration, we will continue recruiting young researchers to develop more promising fields in biology and medicine.”
Last Updated Date : 05/01/2026