Regenerative medicine: Can human organs be grown in a laboratory?
Quite a few creatures are able to regrow their organs- plants, but also animals such as starfish, crabs, certain insects and of course the hydra, which received its name from the mythical monster who fought Hercules and grew three heads for every single head cut off. While tissue renewal, or regeneration, exists in nature at different levels, the question of whether it can be applied in medicine - for example, to grow transplantable organs in the laboratory from single cells- is still being explored.
Dr. Moran Yadid, from the Azrieli Faculty of Medicine and the Dangoor Center for Personalized Medicine at Bar-Ilan University, deals with these exact questions. A biomedical engineer and Technion graduate, Dr. Yadid did her post-doctorate research at the Harvard John A. Paulson School of Engineering and Applied Sciences. She is currently engaged in the development of innovative therapies and human tissue engineering that simulates the functions of various organs- all from her laboratory here at Bar-Ilan.
Regenerative medicine: Medicine aimed at tissue regeneration
Moran, if tissue regeneration exists, why is the damage to the heart after a heart attack considered irreversible?
“The body does indeed have tissues that can regenerate themselves, for example in the skin, liver and bones. Blood cells are also replaced and regenerated all the time. However, most cell types in the human body have limited regeneration capacity or are unable to regenerate at all. This is why after a stroke or heart attack the damage to these organs is irreversible. Regenerative medicine is intended to provide a solution for situations involving damage to such tissues.”
What types of solutions can regenerative medicine offer?
“There are two approaches. One approach deals with the engineering of tissues and organs outside the body - in-vitro, for the purpose of transplanting them into the body. The second approach deals with the self-regeneration mechanisms that can be encouraged within the body. If, for example, someone has a blocked blood vessel so not enough blood is reaching the heart, we would like to encourage the tissue in the body to produce a new blood vessel. There is also a third approach, which is a combination of the previous two. For example, the laboratory produces tissues or a transplantable biological material that encourages the growth and regeneration of the body’s natural tissue. This is called cell and tissue harvesting.”
Heart on a chip?
Dr. Yadid brings her knowledge of tissue engineering and the development of miniaturized organs from her postdoctoral work at Harvard, where she engaged in heart tissue engineering and stem cell and organ-on-chip programming.
Moran, how can you “program” cells?
“Stem cell programming is an innovative technology that was established about a decade ago and for which the Japanese doctor Shinya Yamanaka received the Nobel Prize in 2012. With this technology, you can take a skin biopsy or a blood sample from any person and turn the mature cells into stem cells. It is important to understand that stem cells can basically develop into other types of cells, for example muscle cells. Reprogramming enables skin cells to revert back to their previous state: stem cells with the potential of turning into a wide variety of cells. In other words, it is possible to take a sample of a person’s skin cells, then reprogram them and produce that person’s cardiac muscle cells including all their genetic traits.”
And where does the chip come into the picture?
"’Chip’ is a term taken from the classic silicon chip industry. We call it a chip because we use techniques taken from the world of chips during its production process. What is meant by an organ-on-chip is that we grow miniature human tissue derived from stem cells, thereby reproducing the basic structure and function of the tissue as it is in the body, and we then integrate that tissue into tiny channels containing various sensors that allow us to receive information about the function of the tissue. For example, for heart tissue we have electrical sensors that measure the contraction of the heart and its electrical activity – two decisive factors for normal heart function. This is a heart-on-chip, and it can be designed according to the research question and whatever it is we want to test. The beauty of it is that it is also possible to connect between chips and thus create an organ system on a chip – perhaps in the future we will be able to connect the entire human body-on-chips.”
It sounds amazing, but what is the benefit of this technology?
“This field has grown because of problems with drug development and testing. One of the ways to test the safety and efficacy of a new drug before it reaches human trials is to conduct animal trials. The advantage of such trials is the ability to see the activity of the studied organ within a complete environment, similar to the human body. However, we find that even if the drug is effective in animals, it does not always work as intended in humans, and in some cases may even be dangerous for them.”
And trials in humans are not a trivial thing.
“Exactly, which is why we are trying to test drugs on human cell cultures. For example, testing an obesity drug on a liver cell culture. The disadvantage of doing this is the isolation of these cells from their environment, and the fact there is no reconstruction of the three-dimensional structure of the liver or its extracellular environment. These things are critical for understanding the function of the human organ. Organs-on-chip are an attempt to solve this problem. In the laboratory, we collect data on the activity of the heart and the efficacy of various treatments, whether genetic editing, drugs or biological treatments - and we test all of them on a miniaturized, three-dimensional heart-on-chip.”
In a few years, will organs-on-chip replace the clinical stage in humans in the drug development process?
“The clinical stage in humans is essential, but today organs-on-chip constitute an additional layer between animal trials and this stage. Maybe in the future they will even save us the need for animal trials. About a year ago, the US Senate passed an FDA bill by which animal trials are no longer required in pre-clinical stages - this is a very significant announcement in the field, which validates our decision as researchers to continue working in these directions.”
Do you use the heart-on-a-chip technology here in Israel as well?
“Absolutely. For example, together with Dr. Oshrat Rokach from the Hematology Department at Assuta Hospital we use the heart-on-chip technology to investigate treatments for amyloidosis, a rare disease that causes blood plasma cells to produce masses of proteins that accumulate in the cardiac muscle and lead to heart failure. To date there is no cure for amyloidosis because they have not been able to produce an animal model with this specific pathology to test drugs on. In this case, a human heart-on-chip offers a relevant model system which we hope will yield new insights and potential treatments.”
An incredible machine called the human body
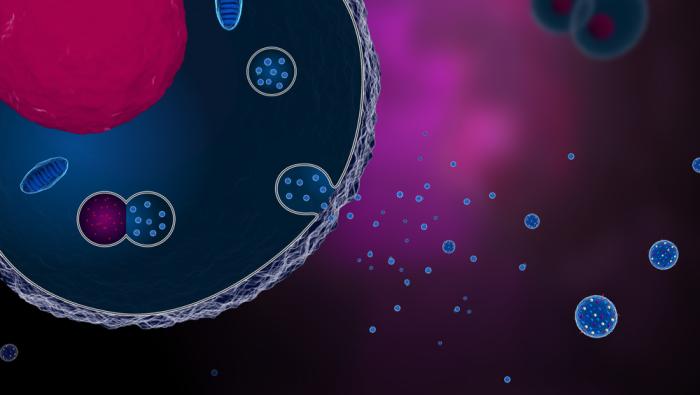
Science naturally evolves over time. Sometimes researchers discover that a certain substance that they had previously thought was unimportant actually performs an important job. This is exactly what happened with extracellular vesicles, also called exosomes. These vesicles are naturally excreted from cells, but for years scientists believed that they were "junk” discarded by cells and did not investigate them thoroughly. It was only in the early 2000s that scientists understood that they have multiple important roles.
Moran, what has been discovered in recent decades about the role of vesicles?
“What scientists discovered is that vesicles transport proteins and nucleic acids, such as DNA and RNA, from one cell to another. They are basically responsible for communication between cells. This communication is reflected in translational changes, such as the production of proteins necessary for the vital activity of cells.”
And what is so special about it?
“It was the first time in history that scientists witnessed the transfer of DNA, a very unstable structure that doesn't just pass through the blood, from one cell to another, in a mammalian animal model. The vesicles, which consist of a stable lipid envelope rich in cholesterol, are like vehicles for nucleic acids. They are excreted from a cell located in a certain area of the body and transport the nucleic acids to another area of the body through the bloodstream.”
Why does the body send vesicles between cells?
“I will give you an example from our research of endothelial cells - cells that line the walls of the heart and blood vessels. What's special about endothelial cells is that they transform the cardiovascular system into a kind of giant organ. Thus, when the body detects inflammation in the cardiovascular system, it sends out vesicles from these cells, whether they are close to or distant from the point of inflammation. Our research has shown that vesicles contain about 1,800 different proteins as well as genetic material and contribute to normal heart function - for example, proteins that can affect the contraction of the cardiac muscle or the reaction of heart cells to stress.”
What vesicles did the doctor prescribe for you today?
Dr. Yadid has an interesting hypothesis regarding the function of the vesicles of the cardiovascular system. In her opinion, there is no dichotomy between suffering from angina pectoris and being completely healthy. At every moment we are at a certain point on the spectrum in relation to having angina pectoris. This means that every day we might experience mild ischemia (micro-ischemia), which is a disturbance in the blood flow to the heart, or an increase in the workload of the heart, but we do not sense it because the vesicles that the endothelium sends produce proteins that allow the heart to function even in this situation.
Moran, can we harness your hypothesis to treat cardiovascular diseases?
“We are investigating whether it is possible to synthesize the vesicles from the endothelium and manufacture them as a drug; for example, as prophylactic medical treatment that can be administered to patients with heart problems. If there is anyone at risk of a heart attack, which is something that can be discovered quite easily these days with the help of artificial intelligence, for example, we will be able to provide them with prophylactic treatment with increased doses of vesicles.”
Let's assume that in the future a heart patient will be prescribed treatment with vesicles - how is this different from the drugs that are taken today?
“Vesicles do not have one essential component, but rather many components that can simultaneously treat different problems in the cardiovascular system. Most drugs can only address one problem; for complicated issues, patients must take a cocktail of drugs which often causes them to discontinue their medical treatment completely. On top of that, we want to know if it is possible to improve the composition of vesicles to better adapt them to the patient and their particular condition.”
So, treating with vesicles is actually personalized medicine?
“That's what we're looking into. Heart diseases are caused by different conditions. Currently, we are focusing on people who have cardiovascular diseases caused by diabetes and obesity. We are investigating what happens to the diabetic heart and how diabetic patients can be administered prophylactic or restorative treatment that is adapted to them, with the help of vesicles, after a heart attack.”
What is "translational research" and who is it intended for?
Recently, Dr. Yadid's laboratory received a grant from the Israel Science Foundation (ISF) for their research of diabetic heart-on-chip. In addition, Moran has received a special grant for the development of infrastructures for a laboratory at Galilee Medical Center in Nahariya.
Moran, why is the research laboratory located in Nahariya and not at Bar-Ilan University?
“Part of the university's concept is that it is important to conduct research within the clinical environment: to see what happens at the medical centers themselves; to establish collaborations; to translate the needs of patients and doctors into research; to test their actual feasibility; and ultimately, to see the research go out and help someone. We call this kind of research ‘translational research’. This results in a significant boost for research in the Galilee region and the medical communities there.”
Can you give an example of how this "translational research" takes form in the field and how it meets actual needs?
“The diabetic heart-on-chip is actually a collaborative endeavor with Dr. Nimrod Rahamimov and Dr. Uri Eyal from Galilee Medical Center. Diabetes is a complex disease that affects all body systems, and unfortunately, we see a high prevalence of diabetes here in the Galilee region. Dr. Eyal is a vascular surgeon, and he treats diabetic patients over time, especially those with vascular complications. Severe cases are transferred to orthopedic departments, where Dr. Rahamimov and other doctors treat patients at advanced disease stages and even amputate limbs of diabetic patients. From amputated ischemic legs we extract the cells needed to research the diabetic heart-on-chip, to better understand the pathological changes that occur with the disease and to develop drugs for patients. Collaboration with the medical community is an actual part of our research.”
Dr. Moran Yadid’s laboratory at Galilee Medical Center is now recruiting doctoral students, in particular doctoral students in the fields of biomedical engineering and electrical engineering.
Last Updated Date : 12/11/2024