"You Are What You Eat – Really?" An Interview with Dr. Lior Lobel on Gut Bacteria and Personalized Medicine

Are you familiar with the phrase, "You are what you eat"? Typically, when people say this, they mean that our food choices affect our energy, health- even our emotions. "That's more or less the focus of my research," explains Dr. Lior Lobel from the Dangoor Center for Personalized Medicine at Bar-Ilan University. "As our diet breaks down into nutrients that are absorbed from the digestive system into the body, the literal interpretation of the phrase implies that we are composed of the same building blocks as the food we consume. In that sense, we indeed are what we eat."
Dr. Lior Lobel investigates how gut bacteria affects human health, with a particular focus on chronic kidney disease and cancer. He completed his doctorate at Tel Aviv University and pursued his postdoctoral fellowship at the Harvard T.H. Chan School of Public Health, where he also served as a fellow at the Cancer Research Institute (CRI). Subsequently, he established his own laboratory at the Faculty of Life Sciences at Bar-Ilan University.
What happens in the gut doesn’t stay in the gut
Dr. Lobel's lab focuses on the triangular relationship between food, gut bacteria and the human body. Since gut bacteria act as intermediaries between the food they break down and cell activity, understanding the mechanism of their action will provide us with knowledge that can advance personalized medical treatments.
Hello, Dr. Lobel. Is it true that bacteria are really a part of the digestive system?
"Not just bacteria. We're talking about the microbiome of the digestive system, which is the` community of microscopic organisms that exist inside of the system. Gut bacteria are one part of the digestive system's microbiome and are integral to the food decomposition processes that occur there."
And you focus specifically on gut bacteria?
"Yes, and there are several reasons for that. The first is numerical: while the stomach contains 102 different organisms, the numbers rise to 105 in the small intestine and really skyrocket to 1011 in the large intestine. What's also interesting about gut bacteria is that they can break down substances that other bacteria, in earlier parts of the digestive system, failed to decompose."
Why is this important?
"As part of these digestive processes, various substances are released, and we would like to understand how these substances affect the digestive system, the immune system, the nervous system and more. Some of these byproducts are absorbed from the intestines into the body through the intestinal lining or pass into the liver via the portal vein. By studying these effects, we can understand how to help patients with various diseases."
Archimedes, behind you: Dr. Lobel’s Eureka moment
The history of science is filled with fascinating discoveries that occurred unexpectedly or in a moment of sudden insight, commonly referred to as a 'Eureka moment". A famous example of this is Archimedes' discovery of the principle of buoyancy while taking a bath. Dr. Lobel also had a Eureka moment, during his postdoctoral studies at the Harvard School of Public Health, and which led him to his current research.
Tell us about that moment. How did it unfold?
"My first project at Harvard was actually a study on nutrition and cancer. We were working with animal models that develop cancer spontaneously. That means you have to wait several months until tumors spontaneously develop in the intestines, and then give them a specific diet to see the effect. Waiting for the tumors takes quite some time, so in the meantime, I read more about the impact of diet on bacteria, even though our lab wasn’t focusing on that. During my PhD, microbiome research gained a lot of popularity, and I was glad to join the field."
And did you discover something?
"While reading the articles, I discovered a surprising gap in the research. There weren’t many studies that examined the impact of a specific diet directly on gut bacteria, and I thought that this could potentially be interesting. This discovery led me to rush to the lab and conduct the experiment myself. The results were published in one of the most prestigious scientific journals - Science. In short, we found that there are two amino acids in our diet that affect the progression of chronic kidney disease, a condition affecting over 800 million people worldwide."
What is this diet?
"It’s a diet rich in cysteine and methionine. These two amino acids are essential building blocks for proteins in the body, and they have been studied in the context of diet and cancer. We tested their direct effect on E. coli bacteria in our intestines. Incidentally, most E. coli in our digestive system is not only harmless but actually lives in symbiosis with us, even aiding digestive processes."
How does a protein-rich diet containing cysteine and methionine affect chronic kidney disease?
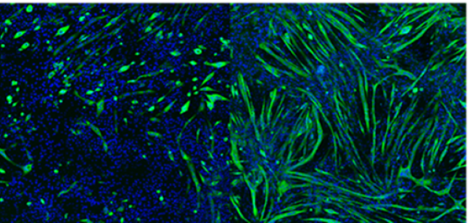
"They inhibit the activity of an enzyme in E. coli called tryptophanase. In all of the experiments, we observed that when cysteine and methionine are added to test tubes with E. coli, the activity of this enzyme decreases."
Is that good or bad for the body?
"It depends. Tryptophanase breaks down a substance called tryptophan, which we receive from our diet. This breakdown process produces a very important product called pyruvate, from which the body can generate energy. However, the reaction also produces another byproduct—indole. In certain conditions, such as chronic kidney disease, indole is toxic to the body. It accumulates in the kidneys and impairs their function. Therefore, a diet rich in methionine and cysteine can help these patients. We proved this in our research and showed that for mice with chronic kidney disease, a diet rich in methionine and cysteine is preferable to a diet poor in these nutrients."
What does this mean for humans?
"Currently, we are still in the pre-clinical stages, conducting experiments in mice. In principle, this could be translated into concrete dietary recommendations, because fish, eggs and poultry are foods rich in these proteins. The problem is that unlike with mice, it is very difficult to control the diet of humans and ensure that they stick to it over time. Therefore, if we discover a drug that can inhibit the activity of tryptophanase in a similar way to how cysteine and methionine naturally do, it could help kidney disease patients."
Coming full circle: What does gut bacteria have to do with cancer?
Earlier, you mentioned that during your postdoctoral research, you studied the connection between diet and cancer, and only by chance did you happen upon the field of microbiota. Now, you're back to studying cancer.
"Today, I am investigating if it is possible to derive information from the activity of gut bacteria in several types of cancer, and if so, how this knowledge can be used to advance cancer research."
Is there a connection between bacteria and cancer?
"The connection between the microbiome and cancer is actually quite astonishing. The assumption today is that about 16% of cancer cases, if not more, develop after an infection with either a viral or bacterial disease. For example, the human papillomavirus, which leads to the development of cervical and other types of cancer, or the bacterium helicobacter pylori, which causes stomach cancer."
Which types of cancer are you studying?
"We are focusing on several different types of cancer simultaneously. We are even investigating the connection between melanoma, a type of skin cancer, and gut bacteria."
How do gut bacteria affect skin cancer?
"Patients with melanoma are treated with immunotherapies, which aim to activate the immune system to fight against the cancer. However, immunotherapies are only effective in some patients, and we don't know why. In 2021, a study led by Dr. Ben Boursi and Dr. Gal Markel from Sheba Medical Center was published, with astounding results. They managed to change a third of a group of melanoma patients who did not respond to the immunotherapy into responders."
How did they do that?
"They showed that transplanting feces from patients who responded to the treatments into those who did not respond caused a third of them to start responding, effectively halting the progression of the disease and even reversing it. Fecal transplants affect the composition and activity of gut bacteria, which has an impact on the immune system. We are collaborating with Dr. Ben Boursi and Dr. Yochai Wolf from Sheba Medical Center to understand which exact change in the composition caused patients to respond to the treatment."
Are you collaborating with other hospitals?
"At the Dangoor Center at Bar-Ilan University, we believe in collaboration. For example, at Sheba Medical Center, we collaborate with Dr. Ben Boursi on prostate cancer research. Together with Northeastern University in Boston we are working on discovering urinary biomarkers for prostate cancer in the microbiome of the urinary tract and prostate. At Ichilov Hospital we have collaborations on research in inflammatory bowel disease, also known as colitis, which affects about 8 million people worldwide. Additionally, we are working in collaboration with other Dangoor Center researchers, such as Prof. Omry Koren, Dr. Nissan Yissachar and Dr. Shai Bel."
Based on the gut bacteria research, what do you now know about personalized medicine and cancer, or about personalized medicine in general?
"It is a fascinating field. If, in the future, we are able predict a patient's response to a specific drug based on their microbiome, we could tailor their treatment accordingly, or even modify their microbiome to match the drug that we want to give them. This knowledge can also be used in cancer research."
So will there be personalized treatments in the future, with fecal transplants for cancer?
"Similar to the case of kidney disease, in these studies as well the goal is to characterize what happens in the digestive processes, so that we can develop drugs similar to the substances released by the gut bacteria and then administer them in a personalized manner to patients. This is another aspect of personalized medicine. I believe that in the future, we will discover more ways that these bacteria influence the body. We are still only at the tip of the iceberg in our knowledge and at the early stages of research, so the field is definitely still unfolding."
Last Updated Date : 12/11/2024